Director: Keith M. Vogt, MD, PhD, FASA
Within our Anesthesiology Residency Program, opportunities for resident-driven research are numerous and broad.

Resident Scholarly Education: Our Facilitation Method
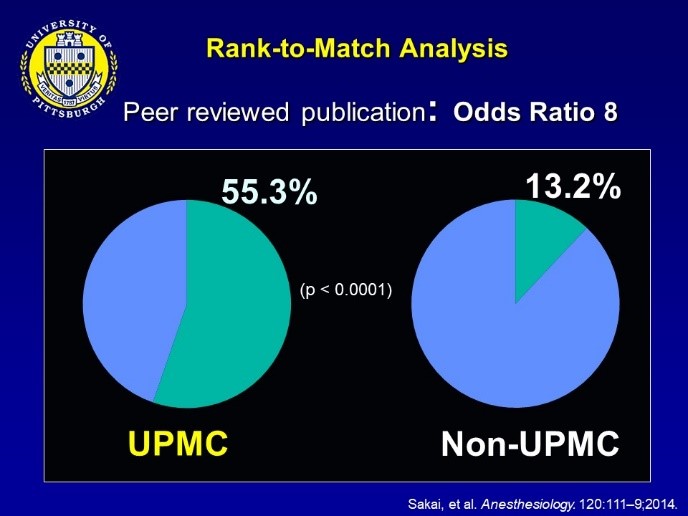 We are active in training the next generation of top researchers. At the same time, we have established a unique resident scholarly activity facilitation system, supporting ALL residents in their scholarly endeavors since 2006. Through the system, our anesthesiology residents have a significantly higher chance of becoming the author of a peer-reviewed publication than the non-UPMC residents.
We are active in training the next generation of top researchers. At the same time, we have established a unique resident scholarly activity facilitation system, supporting ALL residents in their scholarly endeavors since 2006. Through the system, our anesthesiology residents have a significantly higher chance of becoming the author of a peer-reviewed publication than the non-UPMC residents.
PGY-1 (CBY)
We believe that residents can be very productive as part of our CBY program. We encourage an early kick-start of scholarly activity. All CBY interns systematically have the opportunity to launch their scholarly activity during the Anesthesiology Professional Practice (APP) rotation, which occurs in September-October each year. The one-month APP rotation provides a formal curriculum on the principles of research, as well as ample exposure to academic faculty to take advantage of research opportunities and resources formally. The APP rotation has been shown to increase resident engagement in scholarly activity, and many residents have published peer-reviewed articles based on their work done as a CBY resident.
PGY-2 and PGY-3
On-going scholarly educational opportunities (ex. Research PBLD) are provided, and many residents have represented our department at numerous state and national meetings, including the ASA annual meeting. Some residents work with faculty mentors to become primary investigators of Department Educational Seed Grants. Select residents interested in careers in academic research may take up to three months of their ACGME-allowed research time (see details below) during the PGY-2 & PGY-3 years if justified by their research goals.
PGY-4
 Because our residents will have experienced most of the ACGME-required clinical cases by their PGY-4 year, their final residency year schedule is very flexible. An elective Resident Research Rotation (Director: Keith M. Vogt, MD, PhD, FASA) has been very popular, where up to six months can be spent pursuing the answers to clinical or basic science questions. Annually, 20-50% of residents elect this rotation. Some notable resident’ activities during this rotation are:
Because our residents will have experienced most of the ACGME-required clinical cases by their PGY-4 year, their final residency year schedule is very flexible. An elective Resident Research Rotation (Director: Keith M. Vogt, MD, PhD, FASA) has been very popular, where up to six months can be spent pursuing the answers to clinical or basic science questions. Annually, 20-50% of residents elect this rotation. Some notable resident’ activities during this rotation are:
- Richard Hubbard, MD (Class of 2017) spent two months at a pediatric hospital in Bangladesh for a clinical study on the use of surfactant for pediatric respiratory distress syndrome.
- Philip Carullo, MD (Class of 2019) developed and patented a device called the “Esophocculuder” to prevent aspiration pneumonitis at the induction of general anesthesia. He secured a department seed grant and tested the device on a porcine model.
Diverse Research Areas and Active Faculty Mentors
Within this active research environment, interns and residents of all levels are encouraged to participate in projects ranging from basic research, clinical, and translational science (education, simulation, patient safety, QI, and many other areas). Some of the unique features are:
- Active NIH-sponsored research on anesthetic mechanisms utilizes the latest in NMR and MRI technology, headed by Yan Xu, PhD
- We are the administrative home to the Pittsburgh Center for Pain Research, a multidisciplinary effort of basic and clinical scientists engaging in pain mechanism and pain management research.
- We maintain an industry-sponsored Clinical Research Program, with 19 active trials currently in progress.
- Through our strong ties with WISER, residents can work on cutting-edge simulation research.
- As the largest anesthesiology department in the US, our department’s practice management team headed by Mark Hudson, MD, MBA, has won numerous research awards at several annual ASA Practice Management Meetings.
- Functional neuroimaging studies from our perioperative neuroscience research group led to an internationally-recognized resident abstract at the International Anesthesia Research Society annual meeting, with faculty mentors Keith Vogt, MD, PhD, and Jim Ibinson, MD, PhD.
- Perioperative data mining research, mentored by A. Murat Kaynar, MD, MPH, as well as other department faculty, recently led to a resident invited talk and resident abstract award at the Association of University Anesthesiologists annual meeting.
- Educational research, mentored by David Metro, MD, FASA, has led to many resident abstracts and publications.
Resident Scholarly Output
Given our robust scholarly activity support system, our residents have been extremely productive. The following 20 peer-reviewed publications were authored by residents (bold) in 2023-2024:
- Emerick T, Marshall T, Martin TJ, Ririe D. Perioperative considerations for patients exposed to hallucinogens. Reg Anesth Pain Med. 2024 Dec 2;49(12):877-882. doi: 10.1136/rapm-2023-104851. PMID: 38359966; PMCID: PMC11324860.
- Vogt KM, Burlew AC, Simmons MA, Reddy SN, Kozdron CN, Ibinson JW. Neural correlates of systemic lidocaine administration in healthy adults measured by functional MRI: a single arm open label study. Br J Anaesth. 2024 Oct 9:S0007-0912(24)00548-8. doi: 10.1016/j.bja.2024.07.039. Epub ahead of print. PMID: 39438214.
- LaColla L, Nanez MA, Frabitore S, Lavage DR, Warraich N, Luke C, Sultan I, Sadhasivam S, Subramaniam K. Intravenous Methadone versus Intrathecal Morphine as Part of an Enhanced Recovery After Cardiac Surgery Protocol on Postoperative Pain and Outcomes: A Retrospective Cohort Study. J Cardiothorac Vasc Anesth. 2024 Oct;38(10):2314-2323. doi: 10.1053/j.jvca.2024.06.032. Epub 2024 Jul 3. PMID: 39043493.
- Emerick T, Durbhakula S, Eibel MR, Kohan L. Kratom: a primer for pain physicians. Curr Opin Anaesthesiol. 2024 Oct 1;37(5):575-580. doi: 10.1097/ACO.0000000000001413. Epub 2024 Jul 8. PMID: 39011659.
- Tarnasky A, Moghalu T, McNulty C, Shah N, Ibarra A, Orebaugh S. Safety of regional anesthesia for patients with pre-existing ulnar neuropathy undergoing decompressive surgery. Reg Anesth Pain Med. 2024 Aug 19:rapm-2024-105781. doi: 10.1136/rapm-2024-105781. Epub ahead of print. PMID: 39160091.
- Alter BJ, Moses M, DeSensi R, O'Connell B, Bernstein C, McDermott S, Jeong JH, Wasan AD. Hierarchical Clustering Applied to Chronic Pain Drawings Identifies Undiagnosed Fibromyalgia: Implications for Busy Clinical Practice. J Pain. 2024 Jul;25(7):104489. doi: 10.1016/j.jpain.2024.02.003. Epub 2024 Feb 12. PMID: 38354967; PMCID: PMC11180596.
- Tarnasky A, Ludwig J, Bilderback A, Yoder D, Schuster J, Kogan J, Hall D. Trajectory Analysis of Health Care Utilization Before and After Major Surgery. Ann Surg. 2024 Jun 1;279(6):985-992. doi: 10.1097/SLA.0000000000006175. Epub 2023 Dec 12. PMID: 38084596.
- Kocher M, Evankovich M, Lavage DR, Yilmaz S, Sadhasivam S, Visoiu M. Utilizing Peripheral Nerve Blocks for Pain Management in Pediatric Patients during Embolization and Sclerotherapy for Vascular Malformations. Children (Basel). 2024 Mar 20;11(3):368. doi: 10.3390/children11030368. PMID: 38539403; PMCID: PMC10969119.
- Schnetz MP, Reon BJ, Ibinson JW, Kaynar M, Mahajan A, Vogt KM. Bispectral Index Changes Following Boluses of Commonly Used Intravenous Medications During Volatile Anesthesia Identified From Retrospective Data. Anesth Analg. 2024 Mar 1;138(3):635-644. doi: 10.1213/ANE.0000000000006633. Epub 2023 Aug 15. PMID: 37582055; PMCID: PMC10867275.
- Thalla N, Levy I, Pribonic AP, Chauhan G, Srinivasan SK. Dorsal Root Ganglion Stimulation for the Management of Phantom Bladder Pain: A Case Report. Cureus. 2024 Feb 27;16(2):e55043. doi: 10.7759/cureus.55043. PMID: 38550462; PMCID: PMC10977165.
- Verdecchia N, Nelson R, White S, Cladis F. Pre-Admission Oral Clonidine to Reduce Severe Pre-Operative Anxiety in Pediatric Patients with Behavioral Disorders: A Case Series. Children (Basel). 2024 Feb 20;11(3):264. doi: 10.3390/children11030264. PMID: 38539299; PMCID: PMC10969061.
- Paiste HJ, Godwin RC, Smith AD, Berkowitz DE, Melvin RL. Strengths- weaknesses-opportunities-threats analysis of artificial intelligence in anesthesiology and perioperative medicine. Front Digit Health. 2024 Feb 20;6:1316931. doi: 10.3389/fdgth.2024.1316931. PMID: 38444721; PMCID: PMC10912557.
- Solanki PK, Yellapragada S, Lynch B, Eibel M, Viscusi ER, Emerick T. Emergence of xylazine as a public health threat: what does the anesthesiologist need to know for perioperative care? Reg Anesth Pain Med. 2024 Feb 5:rapm-2023-105190. doi: 10.1136/rapm-2023-105190. Epub ahead of print. PMID: 38242642.
- Qiu Y, Hilmi I. The applications of ECMO in liver transplant recipients. Transplant Rev (Orlando). 2024 Jan;38(1):100816. doi: 10.1016/j.trre.2023.100816. Epub 2023 Dec 13. PMID: 38104398.
- Burke HW, Eibel MR, Wang S, Tripp R, Emerick TD. A Transition to Practice Curriculum for Anesthesiology Fellows. A A Pract. 2023 Dec 21;17(12):e01736. doi: 10.1213/XAA.0000000000001736. PMID: 38126884.
- Kaynar AM, Lin C, Sanchez AG, Lavage DR, Monroe A, Zharichenko N, Strassburger M, Saucier K, Groff YJ, Klatt BA, O'Malley MJ, Szigethy E, Wasan AD, Chelly JE. SuRxgWell: study protocol for a randomized controlled trial of telemedicine-based digital cognitive behavioral intervention for high anxiety and depression among patients undergoing elective hip and knee arthroplasty surgery. Trials. 2023 Nov 9;24(1):715. doi: 10.1186/s13063-023-07634-0. PMID: 37946291; PMCID: PMC10634062.
- Pribonic AP, Brancolini SA, Brea F, Cladis FP. Expanded indications of ketamine infusions for pediatric non-surgical pain: a 10 year, single-center experience. Pain Med. 2023 Sep 1;24(9):1111-1113. doi: 10.1093/pm/pnad052. PMID: 37104745.
- Pickle J, Licata S, Lavage D, Visoiu M. Review of bleeding risk associated with prophylactic enoxaparin and indwelling paravertebral catheters: a pediatric retrospective study. Reg Anesth Pain Med. 2023 Jul 6:rapm-2023-104492. doi: 10.1136/rapm-2023-104492. Epub ahead of print. PMID: 37419508.
- Richardson C, Chauhan G, Parrilla FB, Marshall T, Raggi E, Hickey S, Polsunas P, Zhang C, Emerick T. Raising the bar: pain fellowship alumni engagement and the lifelong learner in the post covid era. Pain Med. 2023 Jul 5;24(7):739-742. doi: 10.1093/pm/pnad032. PMID: 36883728.
- Huettner DP, Hahn LK, Noonan Haase MA, Jung FA, Orebaugh SL. Medical Student Instruction in Peripheral Nerve Blockade Utilizing Fresh Cadaver Limbs in a Simulation Center. J Educ Perioper Med. 2023 Apr 1;25(2):E703. doi: 10.46374/volxxv_issue2_Noonan_Haase. PMID: 37377509; PMCID: PMC10291963.
Our residents were authors on the following works presented at ANESTHESIOLOGY (the annual meeting of the American Society of Anesthesiologists), Philadelphia, PA, October 18-22, 2024 (resident names bolded; asterisk indicates presenter names).
- *Guo H, DeMarco N, Brea Parrilla F, Pearce-Smith BA. Difficult Airway in Trauma Patient with Down Syndrome: A Case Report
- *Jin K, Bireley M, Schott NJ. Perioperative Management of High-Risk Caesarean Delivery in a Patient with Moderate to Severe Aortic Stenosis Presenting with Volume Overload and Respiratory Insufficiency
- *Bireley M, Vitale J, Tran T. Sitting Craniotomy in a Pediatric Patient: Perioperative Considerations and Postoperative Pneumocephalus
- *Burlew A, Simmons M, Kozdron C, Ibinson JW, Vogt KM. Effects of Intravenous Lidocaine on Local and Global Connectivity during Resting-State functional MRI
- *Bundock E, Thompson T, Alfaras-Melainis K. Intraoperative Hypothermia and the Potential for Cardiac Arrest
- *Chen H, Best MW. NORA Emergency Management of a Bleeding Difficult Airway
- *Chen H, Yin ZJ, Gelzinis TA. TriClip as Bridge Therapy to Combined Heart-Kidney Transplantation
- *Evankovich Eibel M, Chauhan G. Wireless Peripheral Nerve Stimulation for Chronic Shoulder Pain in a Morbidly Obese Patient on Chronic Anticoagulation
- *Fuller Z, Noonan Haase M, Healy P, Babichenko D, Orebaugh SL. Using Virtual Reality to Teach Residents Peripheral Nerve Blocks
- *Gomez Sanchez A, Brea Parrilla F, Wang D. Simultaneous Double Etiology for Refractory Hypoxia: Dead Space and Shunting
- *Greib J, Alfaras-Melainis K. Suspected Case of LAST Following Bronchoscopy in the ICU
- *Lecker P, Alfaras-Melainis K. Diffuse Desquamating Rash and Multiple Organ Failure Following Ciprofloxacin Administration
- *Lecker P, Massey M, Ungerman E. Acute Right Ventricular Failure and Coronary Artery Perforation Requiring Impella RP
- *Marshall T, Thompson T, Orebaugh SL. Impact of Sciatic Catheter Placements in Fibular Free Flap Donor Sites
- *Minorini R, Ganoza A, Visoiu M. Liposomal Bupivacaine in Preoperative Peripheral Nerve Block for Pediatric Kidney Transplant
- *Mujib W, LaSorda K, Abt J, Aloziem O, Yu X, Alter BA, Lim G. Psychophysical Correlates of Labor Pain in Women with Opioid Use Disorder
- *Oliver M, Wang D. Post-Tussive Cardiac Arrest in a Patient with History of Intraoperative Bradycardic Arrest
- *Paiste H, Lebovitz EE, Profound and Prolonged Isolated Hypoxemia During Vitrectomy under GETA
- *Paiste H, Opitz-Leewe A, Alfaras-Melainis K, Ungerman E. Degos Disease: An Exceedingly Rare Peri-Operative Evaluation
- *Paiste H, Phadke A. Stollings L, Adams P. Pediatric Atrial Myxoma: Previously Healthy Turned Embolic
- *Patel N, Yin ZJ, Gierl B. Difficult Airway Management in Patient with Iatrogenic Esophageal Intubation
- *Puchany A, Lebovitz EE. Anesthetic Management for a Patient with Unknown Mitochondrial Disorder Undergoing MRI
- *Yellapragada S, Solanki P, Lynch B, Evankovich Eibel M, Viscusi E, Emerick TD. The Emergence of Xylazine as a Public Health Threat: What Does the Anesthesiologist Need to Know for Perioperative Care?
- *Puchany P, Alfaras-Melainis K, Shick V. Severe Dysrhythmia and Cardiac Arrest Following Intrathecal Baclofen Pump Replacement: A Case Report
- *Ramirez W, Wang D. Hemodynamic Collapse from Intraoperative Pacemaker Mediated Tachycardia
- *Thompson T, Wang D. Emergence Challenges in Patient with Vocal Cord Dysfunction Undergoing Paraesophageal Hernia Repair
- *Schaefer A, Wang D. Aberrant Right Subclavian Artery: The Culprit of Perceived Intraoperative Hypotension?
- Yin ZJ, *Pham QD, Ungerman E, Whyte A. Aortic Valve Replacement Complicated by Diffuse Coronary Vasospasm
NIH T32 Postdoctoral Research Fellowship
For those looking to pursue research further, we offer an anesthesiology-focused NIH T32 postdoctoral research fellowship for physician-scientists (PI: Yan Xu, PhD). We are one of only 16 anesthesiology programs across the nation with this prestigious NRSA T32 training grant. Select residents have the opportunity to participate in a longitudinal research program that spans residency and postdoctoral research in the Pittsburgh ANesTHEsiology Research (PANTHER) Track offered within our department.
